Jul 01,2022
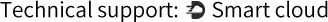
In the rapidly advancing field of clinical diagnostics, accuracy, speed, and sensitivity are not just advantageous — they are essential. Among the most transformative tools in this landscape is the Fluorescence Immunoassay Analyzer , a cutting-edge device that combines the specificity of immunoassays with the high sensitivity of fluorescence detection. This technology has revolutionized the way clinicians detect and quantify biomarkers, hormones, infectious agents, and therapeutic drugs, enabling earlier diagnosis and more effective treatment monitoring.
Unlike traditional colorimetric or chemiluminescent methods, fluorescence-based immunoassays offer superior signal stability, broader dynamic range, and reduced background interference. As a result, Fluorescence Immunoassay Analyzers have become integral to point-of-care testing (POCT), hospital laboratories, and research facilities alike.
Working Principle and Technical Foundation
At its core, a Fluorescence Immunoassay Analyzer operates on the principle of antigen-antibody binding, where fluorescently labeled probes are used to detect specific target molecules within a biological sample. The process typically follows these steps:
- Sample Introduction : A small volume of blood, serum, urine, or saliva is introduced into a disposable test cartridge or microfluidic chip.
- Binding Reaction : The sample flows through a reaction zone containing immobilized capture antibodies or antigens. Target analytes bind specifically to these capture molecules.
- Fluorescent Labeling : Detection antibodies conjugated with fluorescent dyes bind to the captured analyte, forming a sandwich complex.
- Excitation and Emission : The analyzer emits light at a specific excitation wavelength, causing the fluorescent label to emit light at a different, characteristic wavelength.
- Signal Detection and Quantification : Highly sensitive photodetectors measure the emitted fluorescence intensity, which correlates directly with the concentration of the target analyte in the sample.
This methodology allows for ultra-sensitive detection , often down to picogram or even femtogram levels, making it suitable for detecting low-abundance biomarkers critical in early disease diagnosis.
Key Advantages Over Conventional Methods
The adoption of fluorescence immunoassay analyzers in diagnostic settings has been driven by several distinct advantages over older immunoassay technologies:
These advantages make fluorescence immunoassay analyzers particularly well-suited for point-of-care diagnostics , where rapid, reliable results are needed without compromising sensitivity.
Applications Across Medical Fields
The versatility of fluorescence immunoassay analyzers enables their use across a wide array of clinical and research applications:
1. Cardiovascular Diagnostics
Used for measuring cardiac biomarkers such as troponin I, BNP, and CK-MB to aid in the early detection of acute myocardial infarction and heart failure.
2. Infectious Disease Testing
Enables rapid identification of pathogens like influenza, HIV, dengue, and SARS-CoV-2 through antigen or antibody detection, supporting timely isolation and treatment decisions.
3. Hormone and Endocrinology Testing
Facilitates accurate quantification of hormones such as TSH, cortisol, progesterone, and insulin-like growth factors, crucial for diagnosing endocrine disorders.
4. Therapeutic Drug Monitoring (TDM)
Allows precise measurement of drug concentrations (e.g., immunosuppressants, antiepileptics, antibiotics) to optimize dosing and prevent toxicity.
5. Cancer Biomarker Detection
Supports early screening and monitoring of cancers through assays for markers such as PSA, CA-125, CEA, and AFP.
6. Autoimmune and Allergy Testing
Utilized for detecting autoantibodies or allergen-specific IgE, aiding in the diagnosis of conditions like lupus, rheumatoid arthritis, and allergic reactions.
Integration with Smart Diagnostics and Digital Health
Modern fluorescence immunoassay analyzers are increasingly embedded with intelligent features that enhance usability and connectivity:
- Automated Calibration and QC Checks : Reduces operator error and ensures consistent performance.
- Wireless Data Transmission : Enables seamless integration with Laboratory Information Systems (LIS) and electronic health records (EHR).
- Onboard Analytics and AI Interpretation : Some systems incorporate machine learning algorithms to assist in result interpretation and anomaly detection.
- Mobile Compatibility : Portable versions allow for remote diagnostics via smartphone interfaces, expanding access in rural and resource-limited settings.
These innovations align with broader trends toward digital pathology , telemedicine, and decentralized healthcare delivery, reinforcing the role of fluorescence immunoassay analyzers as enablers of next-generation diagnostics.
Challenges and Considerations
Despite their many benefits, the implementation of fluorescence immunoassay analyzers is not without challenges:
- Cost of Equipment and Reagents : High initial investment can be a barrier, especially in low-resource settings.
- Need for Skilled Operators : Although user-friendly, some models still require trained personnel for maintenance and troubleshooting.
- Interference from Sample Components : Autofluorescence or hemolysis in samples may affect assay accuracy if not properly accounted for.
- Standardization and Regulatory Compliance : Ensuring consistency across platforms and adherence to regulatory frameworks like CLIA, CE, and FDA standards remains critical.
Ongoing research focuses on addressing these limitations through improved fluorophore design, enhanced microfluidic integration, and cost-effective disposable cartridges for widespread deployment.
Future Directions and Technological Innovations
Looking ahead, the evolution of fluorescence immunoassay analyzers is poised to follow several promising trajectories:
- Multiplexed Assay Platforms : Development of multi-target assays on a single chip, enabling comprehensive panels from minimal sample volumes.
- Nanoparticle-Enhanced Fluorescence : Use of quantum dots and plasmonic nanoparticles to further boost sensitivity and stability.
- Wearable and Implantable Biosensors : Integration of fluorescence-based sensing into continuous monitoring devices for chronic disease management.
- AI-Driven Predictive Diagnostics : Leveraging real-time data analytics to predict disease progression and treatment outcomes.
- Decentralized and Self-Testing Kits : Expansion into consumer diagnostics with easy-to-use home testing kits supported by mobile apps and cloud connectivity.
These advancements will continue to redefine the boundaries of what is possible in diagnostic medicine, pushing the limits of precision, accessibility, and patient-centered care.


 Español
Español
 Français
Français
 Deutsch
Deutsch
 عربى
عربى